Now you’re living with type 1 diabetes, you would have started using insulin as soon as you were diagnosed. This is to replace the insulin your pancreas no longer makes. Let’s find out more about insulin, including:
Insulin is an essential part of managing your diabetes and will help keep you feeling well.
Managing your diabetes is about finding the right balance. This information will support you to find the skills you need to fit type 1 diabetes into your lifestyle in a way that suits you.
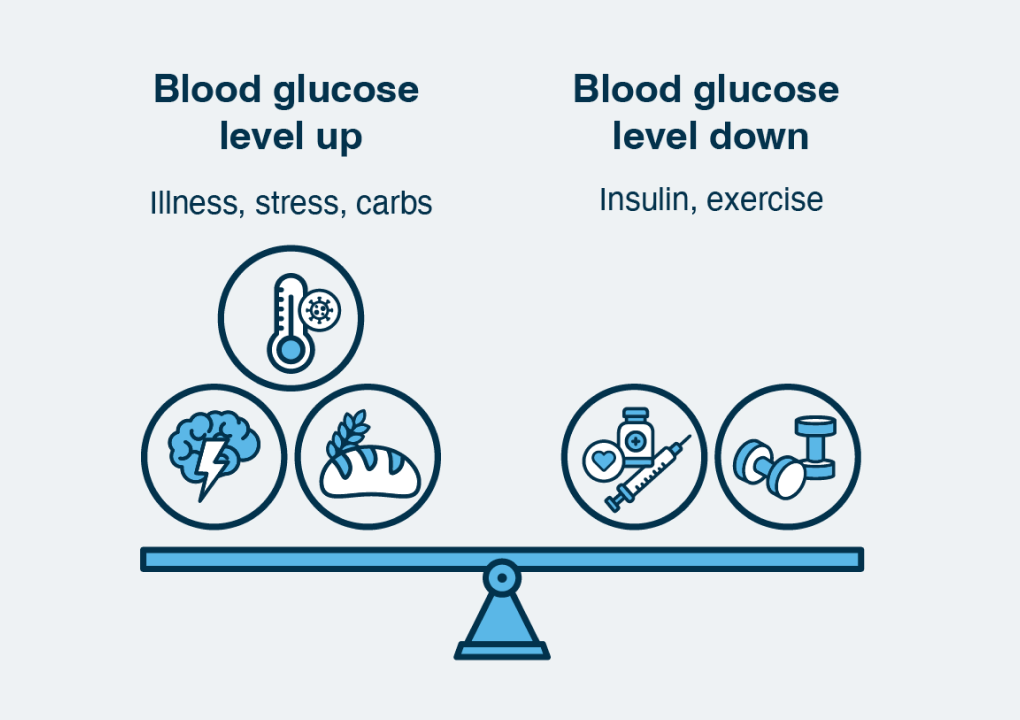
Balancing your blood glucose level means finding out what combination of a balanced eating pattern, being physically active and insulin works for you to keep your blood glucose level in the target range.
This includes things that make your blood glucose level go up, such as the foods you eat, with the things that make it go down, such as insulin.
Everyone with type 1 diabetes needs to replace the insulin their pancreas no longer makes. The easiest way to describe insulin is as a key that unlocks the cells in the body to let glucose in, to be used as fuel or energy. The insulin you use has the same effect as the insulin that was made by your pancreas.
There are several ways to do this. You’ll be able to work with your diabetes health professionals to help you decide which method is best for you. It may be with an:
The method you chose may change in the future; especially as new technology becomes available.
Your diabetes health professionals will help you work out how much insulin you’ll need over the day.
This will be based on your age, lifestyle, and any other health problems you may be living with. Over time both your insulin doses and type of insulin can change.
Insulin needs to be balanced with the carbohydrates (carbs) you eat and drink and your daily physical activity. Sleep, stress, and your general health can also affect your blood glucose level and the insulin needed.

Insulin helps keep your blood glucose level in your target range. Knowing your target range can also help:
Your diabetes doctor (endocrinologist or physician) or diabetes nurse practitioner will work with you to plan the type and amount of insulin you need over the day.
This will also include what to do if your blood glucose level is outside your target range. For example, extra insulin when you’re sick. While there are different brands of insulin, they all fall into three groups:
A basal insulin is a long-acting insulin. It works slowly and is often described as a background insulin. Basal insulin works over 24-36 hours to keep your blood glucose level stable between meals and overnight. It should be taken at the same time each day but doesn’t need to be taken with food.
A bolus insulin is a rapid or short-acting insulin. It works quickly and helps balance your blood glucose level over 2-6 hours. Bolus insulin is given with a meal and sometimes with a snack. The dose is calculated based on the amount of carbs you’ll eat and the blood glucose level. This is called the insulin to carb ratio (ICR). Bolus insulin can also be used to correct a high blood glucose level.

Find out more about the insulin you’re using. Ask your diabetes health professional, for example, how quickly the insulin starts to work after you inject it, how long it lasts in your body, and does it have a peak?
Different sites may cause the insulin to work faster or slower depending on the type of insulin you use. This is the same if you’re using a syringe, insulin pen and pen needles, or an insulin pump.
Insulin is injected into the fatty (subcutaneous) layer under the skin. The more common sites used are the abdomen (tummy) and upper buttocks.
If using arms or thighs, it’s important to avoid injecting into the muscle. The insulin will be absorbed much faster in a muscle, increasing the risk of a hypo.
Talk to your diabetes health professionals about which injection sites you can use.


It’s important to use a new site for every injection or if you’re inserting an insulin pump cannula. This will reduce the risk of lipohypertrophy.
Lipohypertrophy is a firm, fatty lump that appears on the skin. It happens when injecting in the same spot over a long period of time. This changes the appearance of the skin and can also affect how quickly or slowly insulin is absorbed.
Preventing fatty lumps
If you find a fatty lump, avoid using the area until the lump is gone. Talk to your diabetes health professional if you’re worried about your injection sites or if you develop fatty lumps at your injection sites.
Change your pen needle with every injection.
Apply pressure over the injection site with your fingers for 50 seconds after injecting.
Use insulin at room temperature between 4-25 degrees Celsius.
Choose a slightly longer needle length, for example change from a 4 mm to a 5 or 6 mm pen needle.
Find some relaxation techniques such as slow breathing.
An insulin pump is a programmable device, smaller than a smartphone. It uses rapid-acting insulin only. It’s connected through a small plastic cannula that sits under the skin.
Most pumps use tubing to deliver the insulin from the pump to the person. But there’s also a pump that’s tubeless called a pod. Using a pump reduces the number of injections to only one injection every three days.
Pumps are programmed to automatically deliver the basal insulin in small amounts over 24 hours. Bolus insulin is given at mealtimes or when the blood glucose level is above the target range, with the press of a button.
If you decide to use a pump, your diabetes health professionals will:

A pump can give you the right amount of insulin at the time you need it.











Using insulin isn’t just learning to give an insulin injection. It’s also about finding out how to store it safely.

Insulin you’re currently injecting must be stored at room temperature between 16 and 25 degrees Celsius.

Keep your insulin out of direct sunlight in a cool cupboard or cooler bag.

When stored correctly insulin can still be used for up to 28 days out of the refrigerator.

The insulin you’re not currently using is best stored in the non-chilled section of your refrigerator at 2 to 6 degrees Celsius.

When stored correctly, insulin can be used until it’s expiry date.

Check the pack for the expiry date, and don't use it if it’s expired.

Any frozen insulin must be thrown away.